What is
Spina Bifida?
Spina bifida is a congenital neural tube defect (NTD) that occurs during early embryonic development when the neural tube, which forms the baby’s spinal cord and brain, fails to close properly. This condition can affect the spine and spinal cord, leading to a range of physical and neurological problems.
Typically, the neural tube forms early in pregnancy and closes by the 28th day after conception. In babies with spina bifida, a portion of the neural tube doesn’t close all the way. This affects the spinal cord and bones of the spine.
Spina bifida can range from being mild to causing serious disabilities. Symptoms depend on where on the spine the opening is located and how big it is. Symptoms also depend on whether the spinal cord and nerves are involved. When necessary, early treatment for spina bifida involves surgery. However, surgery doesn’t always completely restore lost function.
There are three main types of spina bifida:
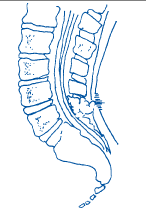
1. Spina Bifida Occulta
This is the mildest form, where there is a small gap in one or more of the vertebrae, but the spinal cord and surrounding structures are usually not affected. Many people with spina bifida occulta may not even be aware that they have the condition, as it often does not cause noticeable symptoms.
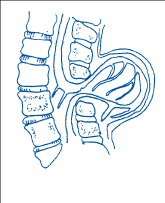
2. Meningocele
In this type, the protective covering of the spinal cord (meninges) pushes through the gap in the vertebrae, forming a sac filled with cerebrospinal fluid. However, the spinal cord itself is not in the sac.
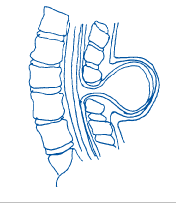
3. Myelomeningocele
Myelomeningocele is the most serious type. It also is known as open spina bifida. The spinal canal is open along several vertebrae in the lower or middle back. Part of the spinal cord, including the spinal cord’s protective covering and spinal nerves, push through this opening at birth, forming a sac on the baby’s back. Tissues and nerves usually are exposed. This makes the baby prone to dangerous infections. This type also may cause loss of movement in the legs, and bladder and bowel dysfunction.
What causes Spina Bifida?
The exact cause of spina bifida is not fully understood, but both genetic and environmental factors may contribute. Folic acid supplementation before and during early pregnancy has been shown to reduce the risk of neural tube defects, including spina bifida.
Treatment
The treatment for spina bifida depends on the severity of the condition and the specific type of spina bifida. Here is an overview of the treatment approaches:
1. Spina Bifida Occulta
- In many cases, no specific treatment is required for spina bifida occulta, as it often does not cause noticeable symptoms.
- Regular medical check-ups may be recommended to monitor for any potential issues.
2. Meningocele
- Surgery is typically required to repair the opening in the spine and close the sac containing the meninges.
- In many cases, individuals with meningocele have a good prognosis, with minimal long-term effects.
3. Myelomeningocele
- Surgery is necessary to close the opening in the spine and place the spinal cord and meninges back into the spinal canal.
- The timing of surgery is often within the first few days to weeks of life.
- In some cases, additional surgeries may be needed to address associated complications or improve function.
- Ongoing medical care and monitoring are essential to manage potential complications, such as hydrocephalus (accumulation of fluid in the brain), Chiari malformation, and orthopedic issues.
4. Ongoing Medical Management
- Children with spina bifida may require ongoing medical care, including regular check-ups with specialists such as neurosurgeons, orthopedic surgeons, urologists, and rehabilitation specialists.
- Physical therapy and occupational therapy may be recommended to help improve mobility, strength, and independence.
- Management of bowel and bladder function is crucial, and individuals may need interventions such as catheterization or medications.
- Assistive devices, such as braces or wheelchairs, may be prescribed to enhance mobility.
5. Hydrocephalus Management
- Hydrocephalus is a common complication in individuals with myelomeningocele. It may require the placement of a shunt to drain excess cerebrospinal fluid and relieve pressure on the brain.
It’s important to note that the specific treatment plan for spina bifida is individualized based on the unique needs and challenges of each person. A multidisciplinary team of healthcare professionals, including neurosurgeons, orthopedic surgeons, urologists, physical therapists, and others, collaborates to provide comprehensive care and support for individuals with spina bifida throughout their lives. Early intervention and ongoing medical management can significantly improve outcomes and quality of life for individuals with spina bifida.
Health Challenges Associated with Spina Bifida
Living with spina bifida can vary widely from person to person, depending on the severity of the condition and the presence of associated complications. Individuals with spina bifida often face unique challenges, but with proper medical care, support, and accommodations, many can lead fulfilling and productive lives. Here are some aspects of life with spina bifida:
1. Medical Care and Interventions
- Regular medical check-ups and interventions are often necessary to address the specific needs associated with spina bifida.
- Surgical procedures may be required to repair the spinal defect, address orthopedic issues, or manage complications like hydrocephalus.
2. Mobility and Independence
- Individuals with spina bifida often face challenges with mobility. The severity can range from difficulty walking to complete paralysis, depending on the level of the spinal cord defect.
- Mobility challenges can vary, ranging from minimal impact to the need for assistive devices like wheelchairs, crutches, or braces.
- Adaptive techniques and assistive technology can enhance independence in daily activities. Assistive devices such as braces, crutches, or wheelchairs may be needed to improve mobility.
3. Orthopedic Complications
- Musculoskeletal issues, such as scoliosis (curvature of the spine), hip dislocation, and joint contractures, are common in individuals with spina bifida.
- Regular orthopedic evaluations and interventions, including surgeries, may be necessary to address these complications.
- Walking to some extent can be accomplished by many children with spina bifida. This is dependent on the location of the myelomeningocele and how well muscles in the legs work.
4. Bladder and Bowel Dysfunction
- Many individuals with spina bifida experience challenges with bladder and bowel control due to nerve damage affecting these functions.
- Management strategies may include catheterization, medications, and bowel management programs.
- Bowel Challenges which may include frequent “accidents” or fecal incontinence due to weak anal sphincter muscles or decreased sensation due to nerve damage. Severe constipation may also occur because waste material moves more slowly through the bowel causing too much water to be absorbed.
- Bowel dysfunction, such as constipation and fecal incontinence, has a significant impact on health, activities of daily living, and quality of life among people with spina bifida. Secondary complications may result from bowel dysfunction and include urologic dysfunction, loss of skin integrity, shunt (hydrocephalus) function, as well as loss of social opportunities and employability.
- Managing bowel function can be one of the biggest challenges accompanying the diagnosis of spina bifida and is also one of the most important.
5. Hydrocephalus
- Hydrocephalus, which is the excess accumulation of cerebrospinal fluid (CSF), affects more than 85% of people with spina bifida. can cause serious damage to the brain impacting its ability to function.
- Treatment often involves the placement of a shunt to drain excess cerebrospinal fluid and manage intracranial pressure.
6. Chiari Malformation
- Some individuals with spina bifida may develop Chiari malformation, where brain tissue extends into the spinal canal. This can cause headaches and other neurological symptoms.
- Surgical intervention may be necessary to address Chiari malformation.
7. Tethered Cord
- Tethered cord syndrome is a rare neurological condition in which the spinal cord is attached (tethered) to the surrounding tissues of the spine. This prevents the spinal cord from moving to keep up with the lengthening of the spine as it grows. Tethered Cord may cause bladder changes (increased urgency and frequency and urinary wetness, urinary infections), bowel changes (urgency and frequency in bowel soiling, changes in stool consistency), back pain, leg and/or foot changes and scoliosis.
8. Skin Issues
- Individuals with spina bifida may be more susceptible to skin problems, such as pressure sores or ulcers, especially in areas subject to prolonged pressure or friction.
9. Neurological Deficits
- Neurological impairments, including weakness, sensory deficits, and paralysis, can result from the spinal cord malformation.
- Rehabilitation and physical therapy may be beneficial in managing and improving function.
10. Education and Employment
- Many individuals with spina bifida pursue education and employment opportunities. Support services, accommodations, and advocacy may be needed to ensure equal access and inclusion.
11. Social and Recreational Activities
- Many individuals with spina bifida engage in social and recreational activities. Adaptive sports, arts, and community involvement can contribute to a rich and fulfilling life.
12. Family and Peer Support
- Support from family and friends is crucial. A strong support system can provide emotional support, assistance with daily tasks, and encouragement.
- Peer support groups allow individuals with spina bifida to connect with others facing similar challenges, share experiences, and offer mutual support.
13. Psychosocial Challenges
- Living with a chronic condition like spina bifida can have psychosocial impacts, including challenges with self-esteem, body image, and mental health.
- Access to support groups, counseling, and other mental health resources can be valuable.
It’s important to note that advancements in medical care and interventions have significantly improved the overall outlook and quality of life for individuals with spina bifida. Early intervention, comprehensive medical management, and a supportive multidisciplinary approach can help address these challenges and enhance the well-being of individuals living with spina bifida. Regular medical check-ups and ongoing care are essential for managing and preventing complications throughout the lifespan.
Spina Bifida
Clinic
A Spina Bifida and Hydrocephalus Clinic is a specialized healthcare facility or program that focuses on providing comprehensive care for individuals who have both spina bifida and hydrocephalus. These clinics are designed to address the unique medical and developmental needs associated with both conditions, offering a multidisciplinary approach to care.
Here are some key points and suggestions for visiting a clinic:
1. Organization of Clinic Reports
Keep clinic reports organized, with the most recent information on top. This makes it easier to track your child’s progress and any changes in their medical status over time.
2. Preparing for Clinic Visits
Before attending a clinic visit, prepare a list of questions you want to ask. This can help ensure that you gather all the necessary information and address any concerns you may have.
3. Taking Notes
Bring a pad of paper and a pen to clinic visits to take notes. The information provided during the visit can be extensive, and having notes can serve as a helpful reference afterward.
4. Communication with Healthcare Providers
Don’t hesitate to ask questions during clinic visits. The more you understand about your child’s condition and treatment, the better equipped you’ll be to provide care.
5. Connecting with Other Parents
Talking to other parents who have children with spina bifida or hydrocephalus can be a valuable resource. They can share their experiences, offer insights, and provide emotional support. If you’re unsure how to approach others, ask the clinic social worker for assistance.
6. Utilizing Community Resources
Explore community service pamphlets and information available in the waiting room. This can give you insights into available support services, programs, and resources for your child.
7. Understanding Recommendations
Pay attention to the list of recommendations provided at the end of each clinic report. These recommendations may include specific actions or follow-up steps that need attention before the next clinic visit.
8. Overcoming Overwhelm
Dealing with a diagnosis of spina bifida and/or hydrocephalus can be overwhelming. Take it one step at a time, and don’t hesitate to reach out to healthcare professionals, support groups, and other parents for guidance and assistance.
Remember, each child’s experience with spina bifida and hydrocephalus is unique, and a collaborative approach involving healthcare providers, parents, and the child can contribute to optimal care and support. Staying informed and seeking community connections can make the journey more manageable.
Living with Spina Bifida & Hydrocephalus
Despite the challenges associated with spina bifida and hydrocephalus, individuals with these conditions can lead fulfilling and positive lives. Here are some positive aspects and strengths often seen in individuals living with spina bifida and hydrocephalus:
1. Resilience and Adaptability
Many individuals with spina bifida and hydrocephalus demonstrate remarkable resilience and adaptability in facing life’s challenges. They develop effective coping strategies and overcome obstacles with determination.
2. Unique Perspectives
Having a different set of experiences can provide individuals with spina bifida and hydrocephalus with unique perspectives on life, fostering creativity, empathy, and a broader understanding of diversity.
3. Supportive Communities
Many individuals with spina bifida and hydrocephalus benefit from supportive communities, including family, friends, and peer groups. These connections offer emotional support and opportunities for shared experiences.
4. Personal Strengths and Achievements
Individuals with spina bifida and hydrocephalus often develop specific strengths, such as problem-solving skills, resilience, and determination. Many achieve personal and professional successes.
5. Advocacy and Awareness
Some individuals become advocates for themselves and others, raising awareness about spina bifida and hydrocephalus. Their efforts contribute to increased understanding, reduced stigma, and improved access to resources.
6. Independence
With advancements in assistive technology and accessibility measures, many individuals with spina bifida and hydrocephalus can achieve a high level of independence in daily activities, education, and work.
7. Strong Support Systems
Having a strong support system, including healthcare professionals, family, and friends, can significantly contribute to positive outcomes and well-being.
8. Educational and Professional Success
Many individuals with spina bifida and hydrocephalus pursue education and professional careers, achieving success in various fields. Inclusive environments and accommodations contribute to their accomplishments.
9. Personal Growth and Development
Living with spina bifida and hydrocephalus often involves continuous personal growth and development. Overcoming challenges fosters resilience, self-advocacy, and a sense of accomplishment.
10. Engagement in Hobbies and Activities
Individuals with spina bifida and hydrocephalus often engage in hobbies, sports, and recreational activities, finding joy and fulfillment in pursuing their passions.
11. Positive Contributions to Society
Many individuals with spina bifida and hydrocephalus make positive contributions to their communities and society at large. Their experiences and perspectives can inspire others and promote inclusivity.
It’s important to recognize and celebrate the strengths and positive aspects of individuals living with spina bifida and hydrocephalus. While acknowledging the challenges, focusing on these positive elements contributes to a more inclusive and supportive understanding of their experiences.